The "Spice" Melange: Exercise, Capsaicin, Cannabinoids, and the Microbiome The "Spice" Melange: Exercise, Capsaicin, Cannabinoids, and the Microbiome
Length: • 9 mins
Annotated by Zakhar
Gut bacteria regulate how much dopamine is released in the brain during exercise.
For decades, Calories In < Calories Out has been the rallying cry of nutritionists and health educators trying to help people lose weight. It’s simple physics, the thinking goes, just burn more calories than you eat, and you’ll lose weight. Unfortunately, the body is complicated. By the time a piece of health advice has been reduced to a pithy four-word saying, it’s lost a lot of important nuance.
For instance, think about how a food’s calorie content is calculated: you put it into a device called a bomb calorimeter, which effectively lights it on fire and measures how much heat you get out. If you did this for every piece of food a person ate in a day, you’d have their “calories in” figure—that’s how much energy they need to burn to maintain or lose weight. But the body’s energy-extraction process isn’t perfectly efficient, which means that exercise isn’t the only source of “calories out” in your life—any calories in your poop are calories that you eat but don’t absorb. It’s long been known (or at least suspected) that we’re missing a big part of that equation, but it’s only recently been explored in depth—partly because solving that problem requires shitting into a bomb calorimeter and lighting it on fire. This is an experiment that it takes a lot of fortitude to propose, let alone carry out. [1]
But people’s biochemical differences pale in comparison to their behavioral ones, so this probably isn’t the most important way your microbiome influences your weight. There’s a good bit of evidence showing that gut bacteria impact food cravings and satiety—so how long a meal keeps you feeling full may be down to your microbiome as well. I could write a whole post series on mechanisms of microbiome <> metabolism interactions, but for today let’s focus on exercise.
Depending who you ask, endurance exercise is either a terrible exhausting chore and proof that god hates us, or it’s the most invigorating way to start your day and get the jump on life. Last week, a fantastic study came out which all but proves that your perspective on the matter depends on your gut bugs: specifically, whether or not your microbiome has a little “kick” to it.
The study didn’t really start out as a microbiome experiment; rather, the researchers’ initial aim was to suss out the factors underlying athleticism more generally. They began by testing the athletic capabilities of nearly 200 mice, both in “forced” conditions (a treadmill test) and “free” conditions (i.e. give them an exercise wheel and see how much they run).
Like people, the mice varied pretty heavily: some were naturally gifted runners, others would wear down after a few minutes on the treadmill. Likewise, their enthusiasm for it was all over the place. While some mice didn’t do any wheel-running at all, one absolute unit ran a full 30-something miles over the course of two days, apparently just for fun. This is especially impressive when you consider how great a distance 30 miles must seem when your body is three inches long.
Analyzing the animals’ genes didn’t turn up much. Ordinarily, lab mice are bred to be as genetically homogeneous as possible, to minimize the influence of inter-individual variability on test results, but the ones used in this study were “outbred” for diversity, because the researchers were hoping to find some associations between exercise performance and natural genetic variations. But, just like in humans, there was no “star athlete” gene for a mouse—so the researchers turned to other parameters, like the microbiome, to see if these could explain the differences.
I’ve said before that, if you’re looking for a biological reason why two people are different along any axis, the microbiome is the logical place to start looking—even before you check the genome. This study bore that out: just by looking at an animal’s gut microbiome, they could get a pretty good idea of what its treadmill performance would be like. Compared to the impact of the gut microbiome, most of the other data they collected (including genetics and behavioral profile) was practically useless as a predictor.
While that predictive power is impressive, it doesn’t let you say “the microbiome causes these differences in exercise performance”, just that it’s associated with the differences. After all, maybe running a lot causes distinct changes in the microbiome. To investigate cause vs. effect, the researchers started manipulating the animals’ microbiomes using antibiotics and fecal transplants.
It worked exactly like you’d expect. Giving a mouse the gut bacteria from a “couch potato” mouse turned it into a couch potato. Giving a mouse the gut bacteria of the 30-mile-runner I mentioned earlier turned it into Marathon Mouse. Across the board, antibiotics worsened performance, which seems to rule out the possibility that some mice are just being bogged down by pathogens. The logical conclusion is that there’s something special in certain microbiomes that confers a crazy athletic drive.
Analyzing the patterns pinpointed a few likely drivers at a species level. To see if these bacteria contained the secret sauce, the group took germ-free mice (which have the same poor exercise performance as ones treated with antibiotics) and “monocolonized” them with samples of these bacteria.
For some of the species they tried, it worked: Colonization with Coprococcus eutactus or Eubacterium rectale put germ-free mice back on par with their healthy-microbiome peers, in terms of endurance. But there were some surprises, too: abundance of bacteria in the genus Ruminococcus was one of the strongest predictors of exercise performance, but mice monocolonized with Ruminococcus gnavus actually did worse on the treadmill than mice which had no bacteria at all.
One potential explanation for this is that R. gnavus might eat the athleticism-enhancing chemicals produced by other bacteria—so you’d find it at high abundance in ecosystems that are full of these compounds, even if it doesn’t contribute to athleticism itself. This would be sort of like how, if you encounter a panda, it’s a safe bet there’s bamboo nearby...but releasing 1000 pandas into a forest will only reduce the amount of bamboo there. It’s also possible that R. gnavus isn’t the right species to achieve that effect, or that it can contribute to exercise performance, but only with the help of other bacteria.
The Spice: Mind Over Matter
The microbiome’s influence on physical performance observed in this study doesn’t seem to be mediated by the things you typically think of when you think about the limiting factors in exercise: things like lactic acid buildup, mitochondrial function, etc. It seems the bacteria are actually increasing the animals’ motivation to keep running.
I’m sure a full 75% of gyms have some variation of the cliché wall sign that says “Whether you think you CAN or think you CAN'T—you’re right”. Turns out, they’ve got a point. When it comes to endurance exercise, your muscles are almost never the real failure point: your willpower is. This is hinted at by the fact that the mice don’t just run more in the forced endurance trial, but also in their free time.
With a couple of very clever experiments, the researchers showed that these performance-enhancing microbes act by increasing the amount of dopamine in critical brain regions during exercise. Some of the techniques they used were fancy and high-tech, like installing a fiber-optic cable and fluorescent dopamine-sensing proteins into the animals' brains, so that they could watch in real time during exercise. Others were less high-tech (like grinding up certain brain regions and measuring the amount of dopamine in them), but still supported the same conclusion: gut bacterial metabolites were preventing the degradation of dopamine in the brain, by reducing levels of the enzyme Monoamine Oxidase A.
So what’s going on here? Is there a tiny red button somewhere in the GI tract labeled ‘‘TURBO’’ that these bacteria are hitting?
Basically, yes. The “button” is a chemo-sensory receptor and the finger that hits it is a molecule, but other than that...pretty much. The researchers found that microbiome-depleted mice could have their exercise performance restored by feeding them capsaicin, a molecule that activates the TRPV1 receptor. Capsaicin is the chemical found in chili peppers, responsible for the sensation of “heat” when you eat spicy foods, and this feeling is mediated by TRPV1.
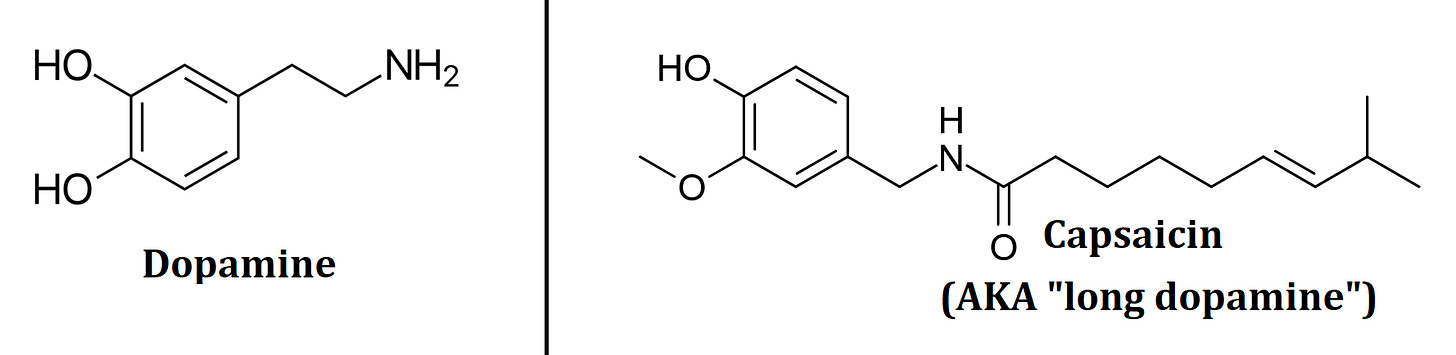
But sensory neurons are multifunctional—they express lots of different receptors, meaning there’s more than one molecular button that can activate them. As it turns out, the bacteria identified in these experiments aren’t hitting the “spicy” receptor
They’re hitting the “dank” receptor.
See, TRPV1-expressing neurons also tend to express a receptor called CB1, which gets its name because it’s activated by cannabinoids and related compounds. The chemicals that gut bacteria produce to increase the dopamine released by exercise are cannabinoid agonists—chemically similar to the endocannabinoids like anandamide that your brain produces on its own.
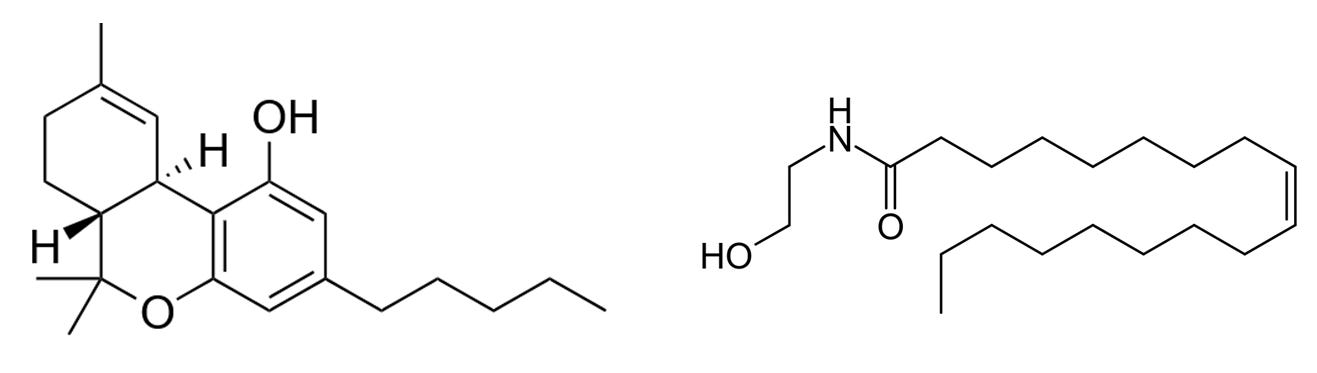
They showed this by treating the animals with antibiotics, which reduced their athletic performance, then feeding them a combination of fatty acid amides like the one shown above—which, like capsaicin, restored their drive to run.
Chemically speaking, these molecules are surprisingly simple to produce: they’re combinations of medium- or long-chain fatty acids, like the ones found in olive oil, and an amino acid or a closely related compound. Because these are “parts” that every living thing has lying around anyway, it makes good sense that they're involved in producing the molecules that signal across kingdoms of life.
The really interesting part of this study, to me, is that these findings probably generalize to things other than exercise. Motivation to build something, make music, or undertake other creative endeavors also relies on dopamine signaling—but those things are harder to measure in a mouse.
So: what are our takeaways, the action items for a human trying to stop hating exercise?
Fish and olive oil in your diet are a good place to start. The most potent cannabinoid mimics typically have unsaturated fatty acids in them, and most bacteria don't produce those on their own—so giving them the chemical building blocks they need is important. (And besides, olive oil is associated with all kinds of positive health outcomes, so it can't hurt.)
But adding the ingredients only helps if you've also got the microbes to work with them at significant levels in your gut. Fortunately, a lot of bacteria are specialized at using one kind of food or another, so eating the right stuff can shift your microbiome substantially, provided you've got some of the right bacteria to start with (most people do).
We’ve got two hints on this front from the paper—Eubacterium rectale and Coprococcus eutactus. The trouble with E. rectale is that there's some evidence that it drives colon cancer development, so maybe trying to encourage its growth isn't the best idea.
So what about C. eutactus? This bug grows well on beta-glucans, polysaccharides that are found in mushrooms, whole grains, seaweeds and lichens [2] . Remember that, when you're trying to change the structure of an ecosystem like the microbiome with selective feeding, it takes time and consistency. Whether or not you should expect to feel an effect is less about “Did I eat mushrooms today?” And more about “What percentage of my meals over the past two weeks have included mushrooms as a substantial component?”
But if you're having trouble mustering the motivation to run, maybe cooking for yourself and incorporating new foods into your diet is a lot to ask. Fortunately, the TRPV1 receptor provides a shortcut, and you can find at least one TRPV agonist on the table at every diner in America: black pepper. And if you ask the waiter, they've probably got hot sauce in the back.
Hmm...whole grains, olive oil, fish, mushrooms, pepper...have we just independently invented the Mediterranean Diet?
I'm generally hesitant to derive health advice from a single study, but in this case, it's fully convergent with a diet plan that's proven to help with weight loss and depression. This is usually a sign that you're on the right track—that you're discovering new reasons to do the things you already knew you ought to.
-🖖🏼💩
Someone’s done it, though, and it turns out that the composition of your gut microbiome does have a significant impact on the percentage of dietary calories you absorb vs. excrete. When I asked, he told me the lab doesn’t smell as bad as you’d expect.
Lichens aren't a typical component of most people's diets, but the study showing that C. eutactus loves β-glucans used a specific one called Lichenan. This is abundant in icelandic moss, which has a long history of use in traditional medicine—so if any readers are feeling experimental but don’t want to change their diets, incorporating this as a supplement would be an interesting thing to try.